Managing Pre-Shift Anxiety as a New Critical Care Nurse
1) The New Nurse Anxiety:
This type of anxiety is simply because you are new, and things are unfamiliar. The unknown can be scary, exciting, and overwhelming. This can show up in ways such as… …what if I don’t know what to do in <insert that one situation here>. …what if I miss something or make a mistake? …I wonder what type of patient I will care for tomorrow! I had pre-shift anxiety for weeks when I started in the Cardiac Cath Lab as a seasoned ICU Nurse. I say this because it is important to understand that this type of pre-shift anxiety isn’t saved for new graduate nurses. It can pop up throughout your career as you do NEW things. You just become more accustomed to recognizing and navigating through it. How to overcome it: Time under tension! You show up, learn more, and do more. Remember the foundations that you already know, call on your resources when you feel overwhelmed, continue to be engaged at work, and put in time outside of work to learn more. With time it SHOULD decrease. That is the expected trajectory of this form of anxiety: a decline with time. If it doesn’t or seems to be ramping up, then you may be experiencing other forms of pre-shift anxiety. (Sarah, how long does this type usually last? Well, everyone is different, but I would say that about the six-month mark of being off orientation is when people *begin* to see this start to fade)2) The Toxic Anxiety:
This anxiety is a result of working in a toxic or unsafe environment. This could be from bullying, lack of support, lack of resources, short-staffed, etc… This form of anxiety may remain the same or increase as time passes. It could be met with other emotions such as fear, sadness, disengagement, or anger. Some examples include… …feeling anxious only when you work with certain people. …feeling dread about going to work out of fear of what you may experience from others or due to the environment. …feeling like you cannot speak up about situations due to retaliation. I experienced this working in a hostile environment where the leader was the bully. It was terrible. I felt like I was walking on eggshells every single day I clocked in. No amount of “deep breathing” was going to help this situation. How to overcome it: I am going to be blunt with you, because I wish someone was with me. Notify the appropriate people, express your concerns to leadership, and address the bully head on. If you attempted taking it “up the chain of command” and it still didn’t improve… then leave. Trust me, it isn’t worth it. Toxic environments take TIME to change. Unless there is strong leadership in making those changes, then it is better to save your mental health. I am all for addressing bullies directly, but sometimes that doesn’t work. Bottom line: know when to cut ties and move on. This type of anxiety can contribute to the last one I want to discuss.3) The Trauma Response:
Critical Care Nurses are exposed to high levels of trauma regularly. It is one reason for our high burnout rates. This type of anxiety is associated with that. It impacts you regularly and interferes with different aspects of your life. I experienced this as an ICU Travel Nurse during COVID, and I know I am not alone in that experience. How to overcome it: It is outside of my scope to advise you on how to manage trauma. However, I will tell you what helped me with mine. First, understanding why I was experiencing it and giving myself some compassion for being human was essential. Other than that: therapy, taking a break from critical care, and having a great support system. Everyone’s response to trauma will be different, but I highly encourage the use of proactive therapy to help process what we witness. I also want to remind you it is okay to leave environments to heal yourself. Remember to Care for the Caretaker.Sometimes these different types of anxieties do not operate in isolation. There may be a combination working together, but it is important to figure out the root of the issue. Without that information, you cannot begin working through it.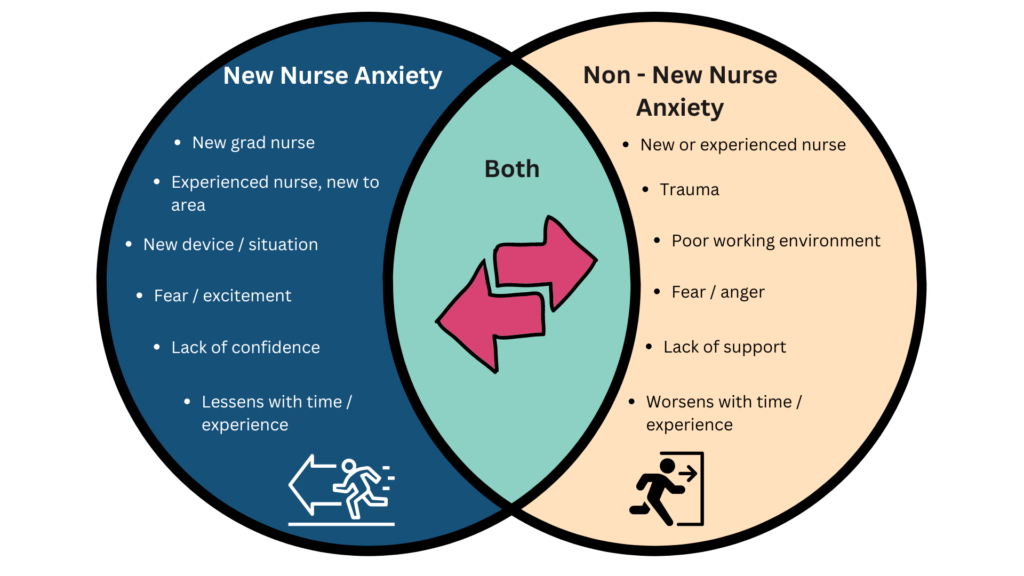
It comes down to two types: one that improves over time, and one that remains constant or gets worse.
If you are experiencing new nurse anxiety, I highly encourage you to lean into it.
If you are experiencing the other forms, then take a moment and reflect on what is best for you as a person. Which may mean leaving the environment and planting roots in one that is geared towards thriving versus simply surviving.
You got this, Sarah