CRRT Terminology for ICU Nurses
Continuous Renal Replacement Therapy (CRRT) remains one of my favorite devices to manage in the ICU, and it was the first device I learned as a new ICU Nurse. Regardless of which subspeciality of ICU you work in, chances are that you will be responsible for learning and performing CRRT. There are three main goals of RRT:

- Removal of excess fluid
- Removal of waste products
- Restore pH and electrolyte balance
CRRT requires ICU nurses to have a good understanding on how the therapy influences acid/base imbalances, electrolytes changes, hemodynamics, volume status, and drug therapy to ensure that it is being performed safely.
If it was one piece of advice for new users to CRRT, it would be to not underestimate the risk involved with this therapy. Managing the device is easy, but understanding how it impacts our patients is a different story.
What is Continuous Renal Replacement Therapy?
A type of renal replacement therapy for critically ill patients who are too unstable to tolerate other modes of RRT such as intermittent hemodialysis (IDH) or prolonged intermittent kidney replacement therapy (PIKRT).
The name gives away a large portion of the benefits of this therapy: it is continuous. This allows for a slower rate, or sometimes zero rate, of fluid removal from patients who are hemodynamically unstable.
I like to use a little bit of math to drive this point across. Say the nephrologist has a goal of removing 1200 ml of fluid from your patient. Refer to the table below to see how that would look with each type of therapy. As you can see, there is a big difference between the three. Now imagine that your patient is on multiple vasoactive medications to barely maintain a MAP > 65.
Which therapy would you feel more comfortable initiating? And if I am being completely honest, sometimes these patients will not tolerate even 50 mL/hr of fluid removal and we are running them positive (don’t worry… I explain what that means below).
| Type of RRT | Uses | Duration | mL/hr if using 1200 mL goal |
| IHD | CKD, hemodynamically stable, acute intoxications, hyperkalemia | 3 – 4 hours per session | 400 – 300 mL/hr |
| PIKRT (ex. SLED) | Critically ill; hemodynamically UNstable; patients who may require multiple interruptions of CRRT d/t procedures | 6 – 12 hours/day | 200 – 100 mL/hr |
| CRRT | Hemodynamically UNstable patients in the ICU | 24 hours/day | 50 mL/hr |
Common terms among all CRRT devices:
There can be additional terminology necessary to understand depending on the device used. However, the terms above stretch across all devices available.
- Patient Fluid Removal: The amount of fluid removed from a patient within a given timeframe. Patients can have orders that either keep patients’ fluid removal goals even, positive (allowing patients to receive volume), or negative (removing fluid). This will be influenced by overall goals of therapy, and patient tolerance.
- Blood Flow Rate: The amount of blood pulled from the patient to circulate through the filter per minute. This value will help determine the speed of solute clearance, impact filter clotting, and influence access/return pressure values.
- Ultrafiltration: The removal of fluid through a semi-permeable membrane. You may see or hear patients receive SCUF therapy. This is Slow Continuous Ultrafiltration. With this mode of therapy, only fluid will be removed. SCUF does not use dialysate or replacement fluids.
- Dialysate: The fluid that is used to exchange solutes within the device filter through the process of diffusion. There can be different concentrations for potassium and calcium. It is important to monitor patient’s lab values routinely while on CRRT to ensure imbalances do not occur, especially if using a lower concentration of dialysate.
- Access: AKA arterial access. This is the line on the circuit that is used to pull blood from the patient to filter, typically this can be identified visually by being the color red. I always remembered access lines by this by thinking “red runs away”
- Venous access: AKA return access. This is the line on the circuit that is returning blood back to the patient. It is usually identified visually by being blue. A little saying I used for the venous access was “blue brings it to the patient”
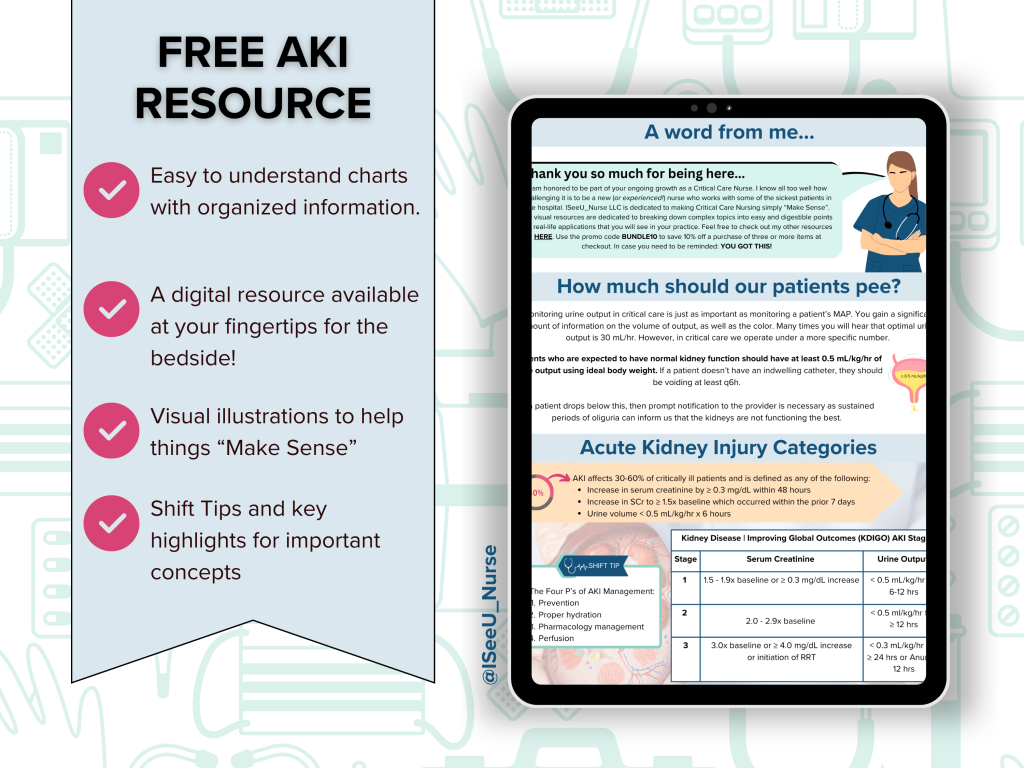
There are different modes of CRRT available on some machines, but we will save that for a different post. Until then, be sure to download your FREE Acute Kidney Injury resource HERE where I cover:
- How much urine is optimal for ICU patients?
- How is an acute kidney injury defined?
- Acute kidney injury categories
- Modes of dialysis summary (more detailed than above table!)
- Temporary hemodialysis catheter review