
Let’s chat about this cool drug that will stain your skin and make your patient’s urine the shade of a Baja Blast. There is only one drug it could be, and that would be good ol’ “Big Blue.” Okay, that isn’t the technical name, just my nickname for methylene blue. If you ever hear me say, “Big Blue coming through,” you will know that things are getting really dicey with my patient assignment.
Methylene blue is one of the new kids on the block…err… new pressor on the pump? When I was your age (cue throwback scene) we didn’t have this drug. So, it was fun to learn about it when I started working with it a few years back. I suspect that the utilization of methylene blue will increase in the years to come due to the data supporting its use in patients experiencing refractory vasodilatory shock, especially septic shock.
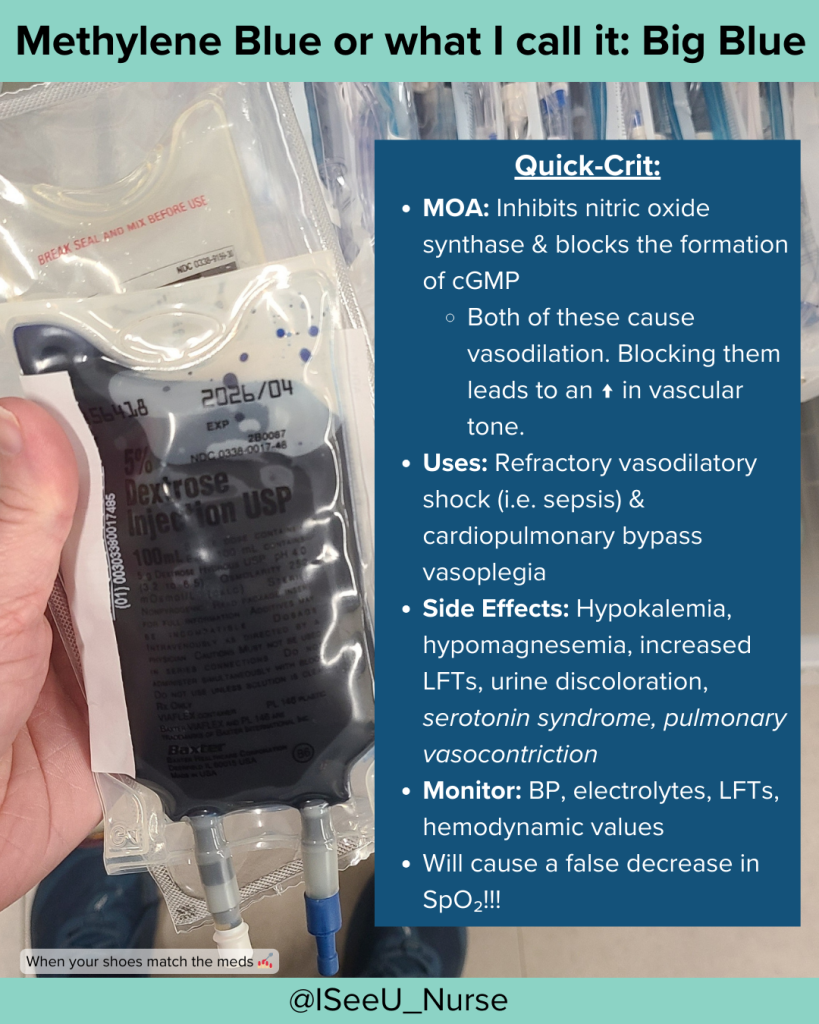
For this blog, we will be reviewing methylene blue and its actions in patients with vasodilatory shock. This drug has been used for years to treat other disorders.
What is Methylene Blue:
Methylene blue is an adjunct medication that supports patients experiencing profound refractory vasodilation. Such as patients in septic shock or in some patients after cardiopulmonary bypass (CPB). In both situations, patients may experience persistent low systemic vascular resistance, aka vasoplegia.
How does Methylene Blue work:
Before you understand the “how it works,” you have to understand some pathophysiology behind vasoplegia:
The release of cytokines and endotoxins stimulates nitric oxide production, a very potent vasodilator. Those two words should ring a bell if you understand septic shock. CPB patients release pro-inflammatory cytokines from various compounding issues, such as blood coming into contact with the CPB circuit, blood loss, surgical trauma, ischemia-reperfusion injury, and endotoxemia.
The production of NO leads to refractory vasodilation, where patients are simply not responding to our traditional vasoactive medications. Not only is NO a potent vasodilator, but it also activates <big word things> that contribute to smooth muscle relaxation, resulting in vasodilation.
This is where Big Blue comes in. Methylene blue inhibits enzyme pathways <nitric oxide synthase and guanylyl cyclase> that contribute to persistent vasodilation.
It doesn’t cause vasoconstriction like other vasopressors (i.e. levophed), but it stops the cascade that causes vasoplegia.
Think of Big Blue as your vasopressor’s buddy who fights off evil so the pressors can press or the body can return to “normal,” thus improving SVR. Like I said, Big Blue comin’ through!
What are the Nursing Considerations with Administration:
1) It will temporarily turn your patient’s urine the color of Baja Blast.

This happens immediately and can last for a few days. It is always interesting to walk down the hall and see the foley bag bright blue/green. It is a tell that the patient received methylene blue.
2) It can cause a false decrease in your patient’s SpO₂ reading.
I had to give Big Blue not too long ago, and I witnessed this firsthand as it was infusing. The patient was pretty sick, and I had about three people in my room before long asking if everything was okay. False readings occur due to how pulse oximetry technology works and the dye’s interference with light transmission.
3) It has a block box warning regarding serotonin syndrome.
Methylene blue can cause serotonin syndrome when combined with SSRIs, SNRIs, MOA inhibitors, or some opioids (i.e. Fentanyl! How many of our patients are receiving this?) Shoutout to our pharmacist.
4) It can cause pulmonary vasoconstriction.
Something to consider if our patient has pulmonary hypertension, or if they have decompensated RV failure. Remember, the right ventricle is a sensitive princess.
The bolus dose:
Methylene blue is an adjunct medication available to support patients with refractory vasodilation. It works by inhibiting enzymatic pathways contributing to persistent vasoplegia, resulting in increased SVR. Your patient’s urine may look like Baha Blast, and the SpO₂ reading might not be accurate. Caution should be used in specific patient populations.

More details about me…
- Founder of The Critical Care Masterclass
- Published writer
- Keynote speaker on various Critical Care topics
- Critical Care Consultant
- Trained and mentored hundreds of New Grad Nurses and countless experienced ICU nurses.
- Assisted with opening up a NSICU in 2021
- Developed a structured program for new CVICU RNs
- Lead in developing a Nurse Residency program for Critical Care
- Professionally Trained Coach
- Playing Big Facilitator Alum Coach
- CCRN & TCAR Certified
Citations:
Alkazemi A, Almoosawy SA, Murad A, Alfares A. Methylene Blue for Septic Shock: A Systematic Review and Meta-analysis of Randomized and Prospective Observational Studies. Journal of Intensive Care Medicine. 2024;0(0). doi:10.1177/08850666241300312
Ballarin RS, Lazzarin T, Zornoff L, Azevedo PS, Pereira FWL, Tanni SE, Minicucci MF. Methylene blue in sepsis and septic shock: a systematic review and meta-analysis. Front Med (Lausanne). 2024 Apr 18;11:1366062. doi: 10.3389/fmed.2024.1366062. PMID: 38698779; PMCID: PMC11063345.
Gutierrez, E. (2023). The vasopressor & inotrope handbook: A practical guide for healthcare professionals. eddyjoemd, LLC.
Ismail A, Semien G, Sharma S, et al. Cardiopulmonary Bypass. [Updated 2024 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482190/
Sari-Yavuz S, Heck-Swain KL, Keller M, Magunia H, Feng YS, Haeberle HA, Wied P, Schlensak C, Rosenberger P, Koeppen M. Methylene blue dosing strategies in critically ill adults with shock-A retrospective cohort study. Front Med (Lausanne). 2022 Oct 28;9:1014276. doi: 10.3389/fmed.2022.1014276. Erratum in: Front Med (Lausanne). 2022 Nov 23;9:1094735. doi: 10.3389/fmed.2022.1094735. PMID: 36388905; PMCID: PMC9650001.
